What matters the most: Mental health at Mac

April 28, 2022
There is a miscommunication between what students want and what Macalester offers in regards to mental health. Mac is providing more resources than it ever has, yet students are often burnt out, anxious, and think –rightfully– that the college can do more about it. It is not a coincidence that the first question in the annual survey sent from student representatives to students themselves, was about the accessibility of mental health services at Mac. Questions two and three were also about mental health resources. Students representatives are asking the right questions and identifying what matters the most at Mac. Yet, there is still a misunderstanding of the nature of students’ demands.
In the meeting held last November after the sit-in, President Rivera mentioned there were available counseling appointments within the next week. One of the immediate steps, if we remember, was to put together a list of resources that Macalester was already offering. There is a narrative, crafted by students and non-students alike, that one main cause of the problem relies on lack of knowledge about what is available. Information travels fast, yet it travels in an impersonal way when there is stigma about the topic. We need to address how information is transmitted, and also the nature of the services themselves: In some cases, disability services act as an intermediary for accommodations which should be universal.
Let’s first talk about information accessibility. If you email the Hamre Center, they will kindly explain the resources available or redirect you to a website. But students want more than that. For classes, we want more than a written description, so we ask our peers the perks about each professor. We need something like that to understand all mental health services at Mac, such as: Press 2, disability services, short-term counseling, group counseling, off-campus counseling through insurance…
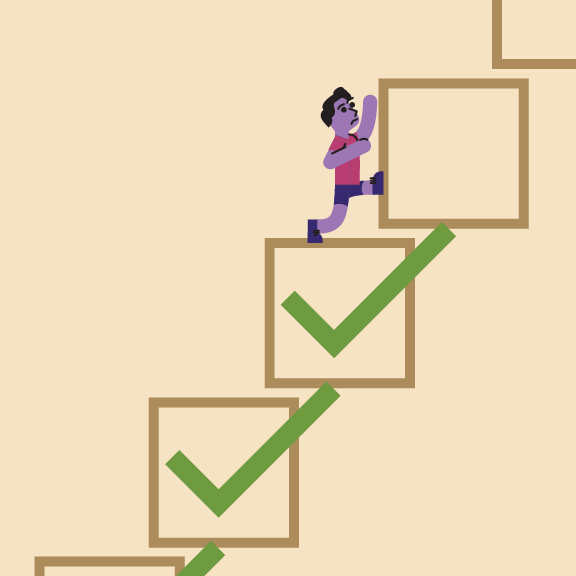
Although students are increasingly open about mental health, we still have a long way to go –many of my peers do not know how to access the services I mentioned above. The answer is therefore to provide active in-person outreach about mental health resources. This must be conducted mainly by staff or students who are fairly compensated. Outreach must happen repeatedly, and not only during orientation. Yes, we need a newsletter about well-being resources. But the key is to make in-person outreach, in order to counterattack the impersonal nature of how we learn about these resources. And when I say outreach, I mean someone going to a class, not a booth that grants zero anonymity or an extra flier in Cafe Mac. Outreach must happen during midterms and before finals, and not only in the first week of orientation for first-years. Sophomores and juniors deserve to hear this info in-person as well. The Hamre Center, the Multicultural Life Dept., and the MAX Center have an opportunity to coordinate outreach efforts to all class years in issues regarding mental health. Outreach will hopefully include Q&As via Instagram and text, reducing the barriers of formal communication.
Now, let’s talk about universal accommodations. If we were to do a survey of how students feel: we would not be well. At best, we would be okay, on average. Being a full-time student amidst the pandemic is mentally exhausting. Even if we are 99% vaccinated and generally very privileged persons, youth have been reporting the highest rates of anxiety and depression across age groups, and throughout history — and that was before the pandemic. How many students are not sleeping because of an exam or an essay on a recurring basis? The answer can not be going to disability services if the problem is a general one. Accommodations regarding flexibility with deadlines and alternative assessments should be clear and universal. People often do not reach disability services because of self-prejudice or because they think they may jeopardize the resources for others. A prior diagnosis of mental health issues plays a role on who is served by disability services, and many folks lack a diagnosis because of the circumstances of their upbringing.
As you are reading this, there are two concerns that arise. One is about universal accommodations, and one is about outreach. Professors may worry that If accommodations are universal, students’ learning will be constrained with take-home exams and malpractice would be harder to control. Let’s be clear: It is up to teachers to figure out how to teach critical skills and information, without aggravating student’s mental health. We reimagined how to both teach and control for COVID transmission rates. Now we need to develop practices to deal with another pandemic that produces suffering and pain in real time: anxiety & depression.
For the “COVID generation”, mental health is an undiagnosed collective crisis that worsens each semester. Scholars will write about this for decades. But we need to do applied research now, because we are the ones living this crisis. A survey must be conducted each midterm and before each final that evaluates student’s mental health. This information should be public, disaggregated by class, and reach the desk of administrators.
Scared about evaluations? We students receive grades all the time. Do not make the survey long, as that is just a barrier to avoid getting the data we want. A question like this will do: “from -5 to +5, how is this class making you feel (being -5 very stressed and +5 very happy)”. Then professors can do a self-survey (from 1 to 5, how much do you think your students are learning?) and average this number with how students measure their own learning (from 1 to 5). The first survey will make teachers accountable to students and administrators about what I hope is a health priority at Macalester. Summing up the results of the first and the second survey would allow teachers to identify how to both care and teach. My anticipation is that the survey results will prove that the trade-off between well-being and learning is more of a myth. As the best educators I know have told me, these two things cannot be separated.
There is a second concern I have not mentioned, the one about outreach. Macalester does not currently have the supply to meet the demand, so it rations its mental health resources. Counselor appointments of 30 minutes every two weeks are, for many, not enough to meet mental health needs. A successful and inclusive outreach campaign from disability services and the Hamre Center would collapse the current resources. But I should not be scared of resources becoming scarce. I want to believe that in such a scenario, Macalester will redistribute resources to respond to the mental health needs that lie below the surface –due to inequalities in diagnosis and stigma around mental health services. My belief is that Hamre center and other departments will want to prove me right, and do in-person and recurrent outreach next year, with anonymous questions before each session.
Outreach and surveys about mental health increase transparency, and give us resources as a community to respond to the mental health needs of students in real time. With outreach, we take the burden off of students with disabilities to seek help – especially to those who have never received professional support before. With class surveys on mental health during midterms, we are reimagining Macalester as a community in which academics and well-being go together, and both students and teachers must be accountable for such balance.






Harold A Maio • Apr 28, 2022 at 6:49 pm
Off on a wrong foot:
—-Macalester will redistribute resources to respond to the mental health needs that lie below the surface –due to inequalities in diagnosis and stigma around mental health services.
Whoever trianed you to accommodate those who say there is a stigma to mental health issues, trained you all too well.